To eradicate any cancer cells that may potentially remain after surgery or chemotherapy, many breast cancer patients also undergo radiation therapy. All patients experience unfortunate side effects including skin irritation, and sometimes peeling and blistering. Patients can also develop permanent discoloration of the skin and thickening of the breast tissue months, or even years, after treatment. There is currently no method to predict the severity of these acute and late effects, and even current evaluation of these effects are based on subjective scoring.
Researchers at the Beckman Laser Institute (
BLI) and Medical Clinic, and the Department of Radiation Oncology at the
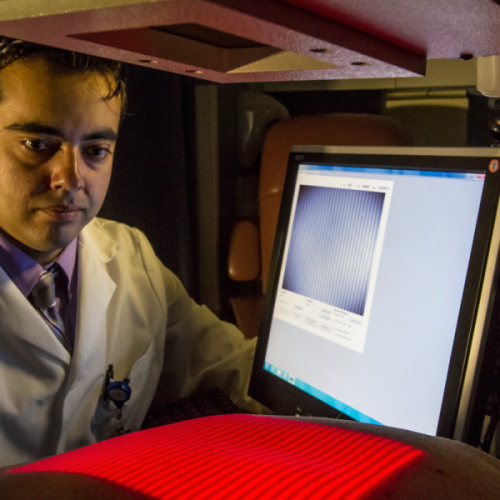
University of California, Irvine are testing a new imaging device developed by start-up, Modulated Imaging Inc. (Irvine, CA). One of these studies is designed to monitor, quantify, and hopefully one day predict skin toxicity levels induced by radiation therapy.
(Image: Modulated Imaging)
“We use visible and near-infrared light at very low power and project it onto the breast,” said Leproux. “We are trying to characterize the skin damage during radiation therapy, especially for the treatment of breast cancer.”
Using their new imaging technique, the project is aimed at using precision measurements to characterize skin toxicity of tissue exposed to radiation. By tracking these measurements throughout treatment, Leproux and her team hope to better understand the factors involved in skin damage and, hopefully, how to predict acute and late toxicities.
“The toxicity is basically the skin damage, a side effect from the radiation,” said Leproux. “There are a wide range of side effects that we’re observing; erythema, hyperpigmentation, discoloration, dry or wet desquamation. Necrosis can happen but is less common.”
Erythema is the formal name for superficial reddening of the skin, and desquamation is skin peeling. Thickening of the skin is a common late side effect.
“The light is shined onto the breast tissue. When interacting with the skin; the light is scattered and some is absorbed,” said Leproux. “The reflected light is detected by a camera. Basically, you’re measuring the absorption and the scattering properties of the tissue.”
More specifically, she and her group use eight different wavelengths of visible and near-infrared light from LEDs, measuring how much of each energy is absorbed by the skin. This provides them with a quantitative values indicative of skin health.
To generate these values accurately, the light from the LEDs is modulated spatially, imparting distinct patterns with a digital micro-mirror device within the instrument. Formally, this functional imaging technique is called Spatial Frequency Domain Imaging, or SFDI.
“Since we use several wavelengths of light, we perform spectroscopy and obtain the content of melanin, tissue hemoglobin, in the de-oxygenated and oxygenated state, from which we can calculate the total blood volume and oxygen saturation in the tissue,” Leproux said. “We measure superficially, about three to five millimeters deep.”
This non-invasive look at just those few millimeters can reveal a lot about the changes radiation induces. Also, because they use a projector technology, they measure over large areas (about 20 cm by 20 cm) without scanning.
“We’re hoping that we can see skin thickening in the scattering parameters we’re looking at,” she said. “We think that the radiation induces a remodeling of the collagen in the skin, which should be seen as a change in the scattering parameter.”
The group did address concerns raised by physicians that the imaging itself exposes the skin to additional radiation, and calculated how their low power device compares to sun exposure. “Ten measurements with our device roughly corresponds to two seconds in the sun,” Leproux said.
Although results are still in their infancy, they show great potential, successfully identifying distinctly different trends in melanin and oxygen saturation over the treatment time.
Along with aiming to one day predict a patient’s reactions to radiation therapy, the group hopes to optimize the device in other ways along the way, perhaps helping to guide the development of better lotions to treat these side effects as well as shrinking the size of the instrument itself.
“We could optimize the current instrument in order to have shorter measurements with a cheaper device. That’s something we’ll look into,” said Leproux.





 CN
TW
EN
CN
TW
EN