It was 1950 when Mr. Hopkins met Dr. Hugh Gainsborough, a gatroentreroligst at St. George’s Hospital London, where he was put forth with a challenge of illumination while operating within abdomen. By 1954, Hopkins invented flexible glass rods which transmitted light from external light source to the inspecting tissue residing within the body of patient, which came to be known as rod lens system. Concurrently early 1950 saw the birth of fibre optic light transmitting system which revolutionized the field of communication.
The current perspective of medical imaging can be distinguished primarily into two techniques.First is interpreting information retrospectively, for example: radiology images, capsule endoscopy and pathology. While second is recording the real time data, for example: Flexible endoscopy, Laparoscopy, Ultrasonography, Ophthalmology and Gynaecology.
The Need:
-
Tissue imaging in medical field is required for the following reasons:
-
Check any abnormal growth (eg. tumors),
-
Biopsy which involves the removal of tissue in order to examine some disease,
-
Women who are facing pregnancy complications,
-
Damage to the internal organs,
-
Bleeding occuring in the digestive tract.
-
Blockage in the arteries of the heart.
The internal tissue imaging could be through a procedure known as Minimal Invasive Surgery (MIS); where the doctors do not get the line of sight view of tissue to be investigated. So a device equipped with CCD camera needs to be reached near the subjected tissue for its imaging and hence its inspection. Having a better MIS would mean that the patient undergoes minimal trauma and operation recovery time is reduced.
 |
 |
|
Fig1 : A flexible endoscope (All image courtesy belong to Wikipedia.org) |
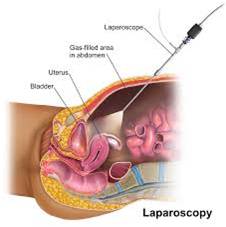
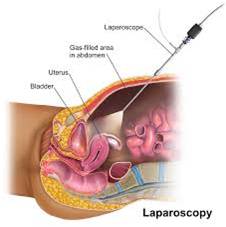
Fig2 : Illustration of laproscopy |
Minimal invasive surgery primarily includes Endoscopy and Laparoscopy surgery. Endoscopy is a procedure through which the physician inserts a flexible and thin tube (as shown in Fig 1) via mouth all the way to stomach, duodenum and esophagus which could be imaged using a monitor. While in Laparoscopy an incision (0.5 to 1.5cm) needs to be created through abdomen itself (as shown in Fig 2) to probe the flexible endoscope within. In Laparoscopy the physician gets direct visualization of complete abdominal area. The Laparoscopy inspection could also extend to areas covering ovaries and some exterior parts of the uterus for examining women who are facing complications in pregnancy.
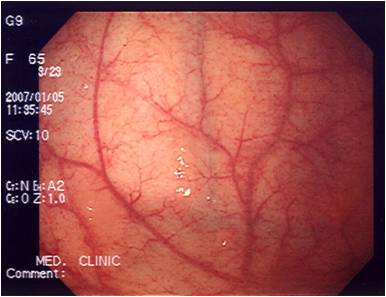
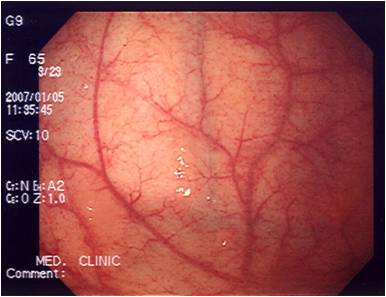
Fig. 3 shows the endoscopic images of stomach, where one can interpret blockages and bleeding area if any.
 |
|
Fig.3 Image of a normal stomach. |
Present Illumination solution:
The present standard light source for most of MIS is Xenon based arc lamp, which emits a broad range of spectrum across the visible range which is very close to that of day light. Xenon lamps are high powered and highly inefficient as it requires round about 300W of electrical power to delivery just about 1W of optical power. The need of illumination is one of the major prerequisite in endoscopy, because if lux level on the inspected area is lower than threshold, the image captured may get distorted and hence resulting in erroneous result.
Alternate source include laser based phosphor fibres and supercontinuum lasers, but these works in niche area and generally for a narrow illumination area such as a focused area of cancer or tumours surgery (which require high lux levels within a small coverage of area). While LED’s which have many advantages are slowly being introduced in the field of medical imagining, mainly because of its miniature size and flexibility in its arrangement. The arc based lamps also needs to be replaced every 500 hours, while LEDs work for 50,000 hours. Electronic circuitry of LED that is the driver’s life takes utmost importance. LED’s can produce 1,00,000 lux of illumination on operation theatre table.
The present lighting solution which deals with use of arc based lamps has ergonomic challenges, lower efficiency and inability to create variety of colour (such as violet colour which is required to spot a particular disease, as discussed later). In this regard the new generation of lighting solution is delivered by compact, inexpensive and durable High Brightness Light Emitting Diode (LED) which are having better ergonomic viability.
Recent work of endoscopy using LED’s:
The work by Neil Clancy et al. combines the use of four ultraband LEDs namely red, green, blue and violet spectral regions. A light pipe multiplexer combines these four different lights, which are having a lambertian intensity profile and couples it into a single light cable yielding a manually configurable white light at the other end. The coupling process is the key to this technology, as it may lead to high amount of loss, if coupling doesn’t happen in a proper manner. When used with a white balanced camera, though the output of the light source of LED (0.61W) is less as compared to Xenon (1.5W), but LED’s have the advantage of adjusting to relative intensities which enables contrast enhancement required for different kinds of biological tissue imaging.
The crux of above research was that one can have a while light of varying colour temperature and can be adjusted to the illumination standard that of daylight or xenon lamps. By setting up the spectrum to blue-green region (10 and 30 nm wide respectively), the contrast of the images of tissue is increased by using light that has penetrated superficially into tissue (with depth of less than 200 µm3) and strongly absorbed by blood. The fluorescence imaging of protoporphyrins (which is used as a carrier molecule for divalent cations) is made possible for photodynamic diagnosis in case of bladder cancer detection by using the violet LED.
Whereas the light from LED based systems was found to be more uniform at the distance of 4cm, as stated by Alex C. et al. As compared to the arc based lamps, the shadows were also sharper (16 vs. 44 pixels), the overall mean image intensity was higher (127 vs. 100 arbitrary units) despite of lower radiometric power. The illumination was found to be more stable and less flickering (0.02% vs. 5%).
Future Technologies:
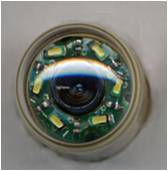
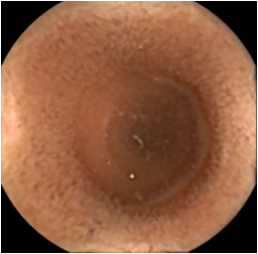
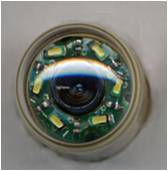
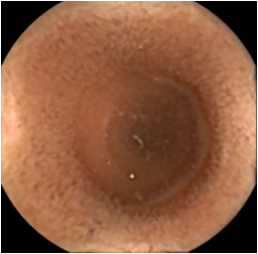
A non invasive technology known as capsule endoscopy incubates a camera and LED within (as shown in the Fig. 4 & 5). The patient in this procedure needs to swallow a capsule, while the camera captures images as it travels along the gastrointestinal tract. The main use of capsule endoscopy is to inspect the upper alimentary track including small intestine which cannot be visualized by other endoscopy methods. It uses Bluetooth to transfer the live stream of captured images to a monitoring system. The challenge foreseen for this technology is the retention of the capsule inside the patient’s body. Fig 6 showcases the intestinal image acquired by the moving capsule endoscope (as explained at a later stage) while moving through the gastrointestinal tract to the intestine.
 |
 |
 |
|
Fig 4: Image of capsule endoscope |
Fig 5: Endoscopic capsule end-on, showing six LEDs and camera lens. |
Fig 6: Image of intestine acquired by capsule technology |
The future of LED based endoscopy seems to be bright, but yet serious research efforts needs to be focused on how the light coupling is improved between reflected light from inspecting tissue and CCD of the camera, electrical to light power conversion efficiency, miniaturizing the endoscope and optimization of illumination.
(Author: Uttam M. Pal is a Technology Analyst at De Core Science & Technologies Ltd., India. He completed his masters from Electrical Dept., IIT Bombay and since working here. His field of interest lie in Photonics, Biology and Semiconductor physics. He can be reached at upa@dstlworld.com.)